In honour of Diabetes Awareness Month, we’re shedding light on diabetes, a condition affecting millions across Canada. Diabetes is a complex and widespread issue in Canada, with type 2 diabetes accounting for 90% of cases, followed by type 1 at 9%, and gestational diabetes at less than 1%. Although each type has unique causes, prognoses, and treatments, all share a common factor: either the body does not produce enough insulin or cannot effectively use it. Today, about 3 million Canadians—8.9% of the population—have received a diabetes diagnosis, with cases climbing by 3.3% annually even when adjusting for population age. Additionally, 6.1% of Canadian adults have prediabetes, increasing their risk of type 2 diabetes. Globally, the rising prevalence of diabetes continues to place an enormous toll on inviduals, families, and healthcare systems, underscoring the importance of awareness, as emphasized by the World Health Organization.
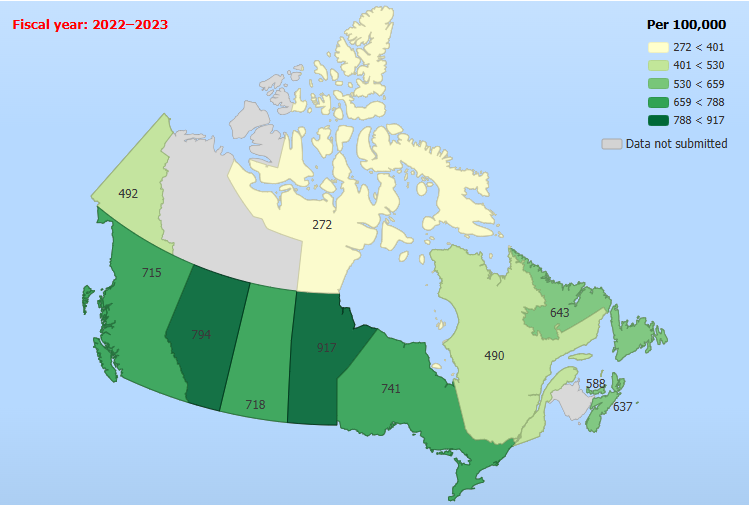
Diabetes mellitus, excluding gestional diabetes, age-standardized incidence rate per 100K, both sexes, age 1 and older
This graph shows age-adjusted diabetes rates across Canadian provinces, highlighting ongoing disparities in prevalence.
The provincial approval processes for diabetes medications in Canada determine access but are inconsistent, resulting in unequal coverage and treatment delays that impact long-term health. Diabetes Canada advocates for a faster approval system to ensure timely access to treatments nationwide.
For example, British Columbians are 13% less likely than residents of other provinces to receive medication within the first month of diagnosis, while Manitobans are 47% more likely. These disparities highlight the need for a streamlined approval process to ensure equitable access to medications nationwide.
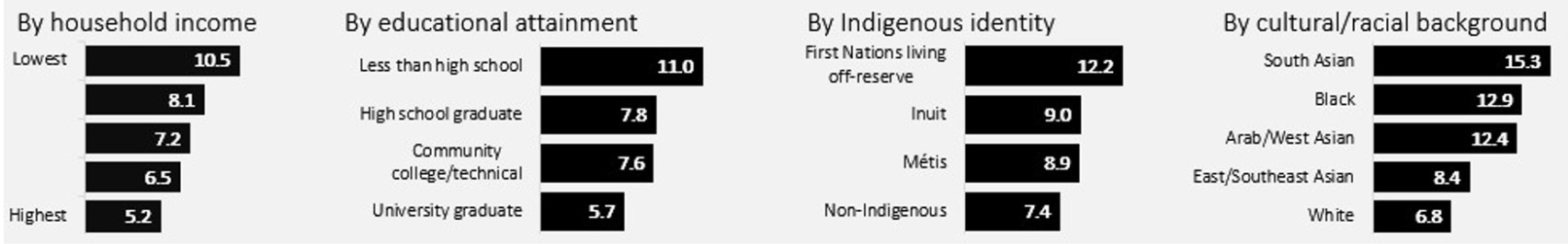
The graph above shows the prevalence rates of diabetes among adults over 18, broken down by Indigenous identity and cultural background. Type 2 diabetes incidence is significantly higher in Black communities—double that of White Canadians—and three times higher in South Asian and First Nations communities. A recent report found that First Nations children in Manitoba are diagnosed at a rate 25 times higher than their non-Indigenous peers. Contributing factors, including limited education, poverty, and inadequate living conditions linked to low income, play a significant role in poorer health outcomes. These challenges are particularly widespread in Indigenous communities, leading to higher rates of chronic diseases such as diabetes.
Among adults, diabetes rates are 2.1 times higher in the lowest income groups compared to the highest. Adults without a high school diploma have a diabetes prevalence 1.9 times higher than those with a university education. Additional contributing factors include limited access to healthcare services, cultural differences in diet and lifestyle, and historical and systemic issues impacting Indigenous and minority communities.
In healthcare, accurate disease diagnosis is essential. However, disparities in diabetes diagnosis and treatment rates persist nationwide, affecting patient care and the allocation of healthcare resources. These discrepancies highlight the urgent need for reliable data insights. Leveraging these insights enables healthcare providers, policymakers, and analysts to identify regional and demographic variations in diabetes diagnoses, paving the way for targeted interventions and better public health outcomes.
Check out our other blogs on healthcare here!